Novel Measure for Prolapse
For my Postural Restoration Certification I had to review a number of Journal Articles and interpret the article through a PRI "lens" I thought this article was too cool not to share. I have edited it from my original submission to make the language a bit more accessible to non-PRI folks as I think this type of study has huge and important implications for guiding practice and research into PRI concepts
ARTICLE:
A novel measurement of pelvic floor cross-sectional area in older and younger women with and without prolapse
Full Citation:
Sammarco AG, Sheyn DD, Krantz TE, Olivera CK, Rodrigues AA, Kobernik MEK, Masteling M, Delancey JO. A novel measurement of pelvic floor cross-sectional area in older and younger women with and without prolapse. Am J Obstet Gynecol. 2019 Nov;221(5):521.e1-521.e7. doi: 10.1016/j.ajog.2019.08.001. Epub 2019 Aug 8. PMID: 31401263; PMCID: PMC6829060.
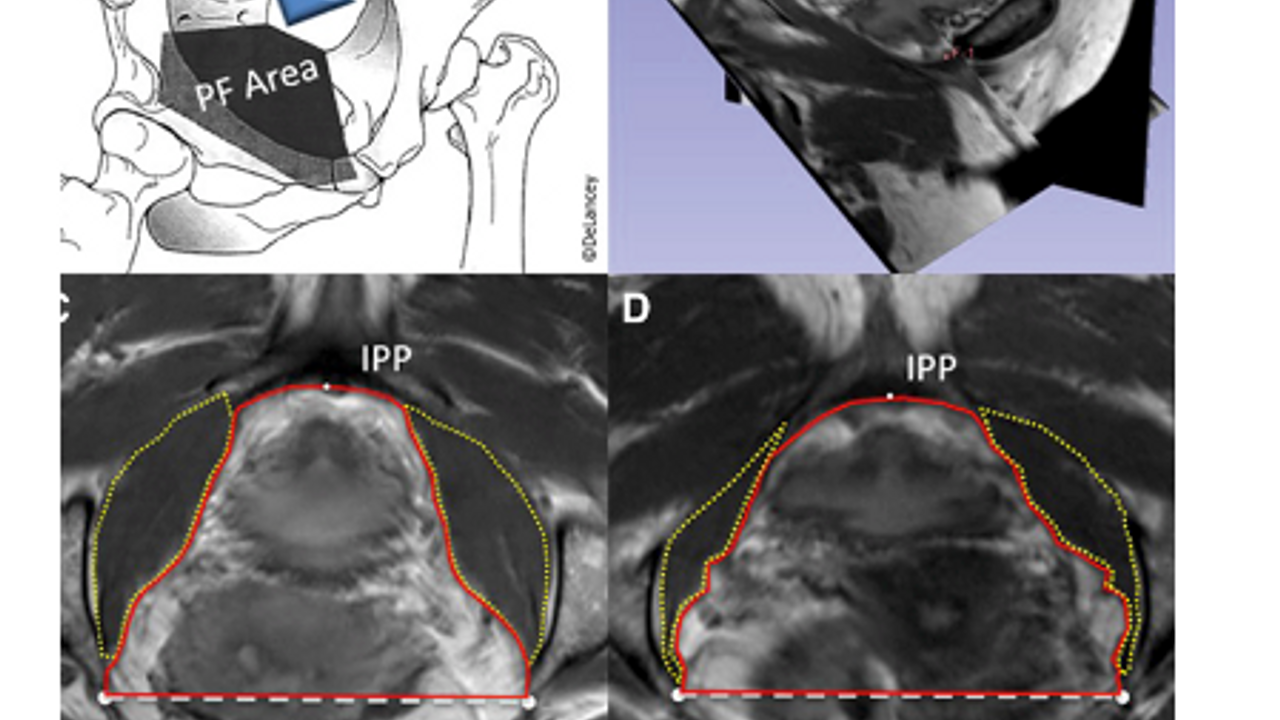
In this study, they ventured to use MRI to study BOTH the anterior pelvic outlet size, and the size of the anterior fibers of the obturator internis muscles in younger population without prolapse, older population without prolapse and older population with prolapse.
These types of imaging studies are very exciting as the postural tendencies and patterns of individuals can start to be seen more clearly vs simple pelvic floor muscle exams or muscle EMG which is non-specific.
One of the theories presented here was that if there is an increased area of the anterior pelvic floor and a decrease in OI size, which helps support the anterior pelvic floor it could help predict prolapse, and may also help with the understanding of the patho mechanics of prolapse. They postulated that if the muscles were spread over a greater area they would not be as effective at managing IAP thus increasing pressure downward on the organs to which I totally agree. Eccentrically oriented pelvic floor muscles do not have the lifting power of neutral/concentrically oriented muscles.

They used intra-spinous distance and measures of cross sectional area of the anterior outlet and OI muscle in the imaging analysis and found that older women with prolapse had a significantly greater anterior outlet size, and a greater intra-spinous distance. They found that older women with prolapse tended to see a trend towards decreased OI size, but it did not reach significance despite the increased anterior outlet size of older women with prolapse.
In PRI there are some typical noted "patterns" of compensation. One of the most common patterns of compensation that I see with individuals with pelvic floor dysfunction is called a PEC pattern. In this pattern we make assumptions about the length tension relationships of muscles in the pelvic floor based on objective testing of pelvic position and ROM. In the PEC pattern the anterior pelvic floor muscles as well as the obturator interni are in a disadvantaged position to work. They are lengthened in this pattern, and so less able to oppose the force of IAP from the abdomen above. Clinically I see clients in this pattern of all ages, and it is a typical pattern to find those with symptomatic prolapse in.
Something I wish they had taken a look at in the study was the posterior pelvic floor/outlet . They stated that posterior border of the sacro spinous ligament and sacrum were not expected to have age related changes and so they did not measure that space in this study. I think clinically this could be incredibly relevant as increased concentric orientation if the posterior outlet could be connected to hemorrhoids, constipation or other posterior wall prolapse(enterocele or rectocele) . Another metric that I think would have been very interesting would have been to compare size and muscle bulk left to right. Asymmetrical patterning is incredibly common and often underlines these more bilateral patterns. Being able to dive into these patterns with an imaging study would be very interesting!
This would also be a very exciting way to test pre and post test PRI treatment effect on pelvic floor function as I feel like we would likely see a change in the anterior outlet area and infra spinous distance as position improved. Clinically I see individuals with highly symptomatic prolapse become symptom free as they move out of these pattern, which then hypothetically, is changing the outlet size and increasing OI muscle bulk, but outside of my internal exam and PRI testing I don't have a clear way to "prove it" which something like this imaging would be able to do!
Overall I think this study is a great representation as to why we need to understand length tension relationships and the position of the pelvis AND the pelvic floor as is relates to being able to manage IAP and pelvic floor muscle activation effectively across the pelvic floor, minimize prolapse risk, as well as treat prolapse conservatively.

